Neuromuscular Therapy for Temporomandibular Joint Disorders and Headaches
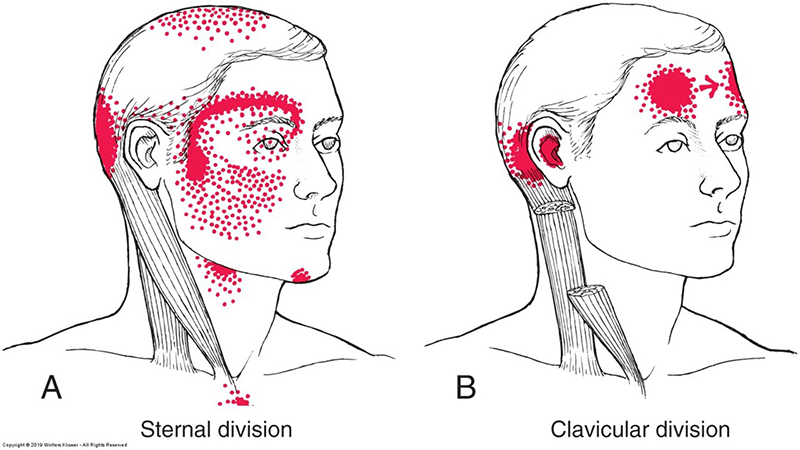
Trigger Points of the Sternocleidomastoid (SCM)
As National Migraine & Headache Awareness month continues, Phil Okazaki, Senior Advanced Neuromuscular Therapy Program Instructor presents a sneak peek into Neuromuscular Therapy for Temporomandibular Joint Disorders and Headaches. To learn more about Neuromuscular Therapy treatments for TMJ Disorders, collaboration with Health Care Providers, and to delve deeper into the biopsychosocial aspects of TMJD and its relationship with headaches, join Advanced Neuromuscular Therapy Program Founder Cynthia Ribeiro for the Online ANMT Program Sampler Class – Temporomandibular Joint (TMJ) Disorder on Thursday, June 24th from 5pm – 8pm.
The Temporomandibular Joint (TMJ)
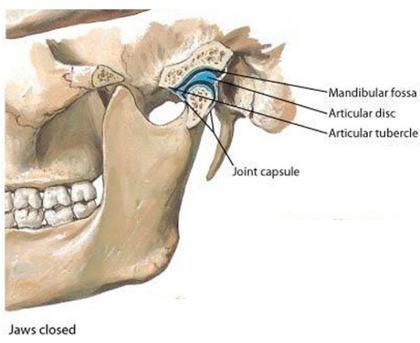
Lateral Temporomandibular Joint (TMJ) Joint Capsule
The temporomandibular joint is the connection of the jaw with the skull. “Tempero” refers to the temporal bone; “mandibular” is the mandible or jaw. The articular fossa is an indentation of the temporal bone located just in front of the ear. The mandibular condyle, the most posterior portion of the mandible, has a rounded top which fits into that indentation. This joint is divided into two cavities by an articular disc. The articular disc is a fibrous structure that can be found between the two articular surfaces; it is a bit smaller and resembles the shape of a lifesaver candy; instead of a hole in the center, there is a thin fibrous material which gets thicker around the edges. This allows the disc to be seated onto the condyle and to be carried forward by the condyle as it translate during movements of the jaw. The disc articulates with the mandibular fossa and the mandible. This disc is attached to the condyle of the mandible by medial and lateral collateral ligaments; the posterior portion is attached to the mandibular fossa by retrodiscal tissue, and the anterior portion is attached to the superior portion of the lateral pterygoid muscle.
These structures, along with the muscles that affect the joint allow for mandibular depression, elevation, lateral deviation (which occurs bilaterally), retrusion (overbite), and protrusion (under bite). A combination of all these movements allow us to use the temporomandibular joint while we talk and chew.
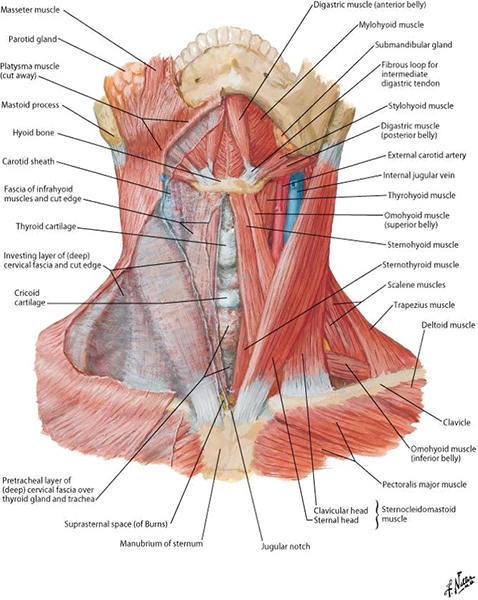
Anterior Neck Muscles
Suprahyoid muscles including the digastic, stylohyoid, mylohyoid, and geniohyoid along with the platysma open our jaw (mandibular depression). To close our jaw (mandibular elevation), we use temporalis, masseter, and medial pterygoid. The side to side motions of the mandible are produced by the lateral pterygoid. Finally the forward (protrusion) and backward (retrusion) of the jaw are executed by the lateral pterygoid and medial pterygoid respectfully.
Temporomandibular Joint Disorders (TMJD)
Temporomandibular Joint Disorders (TMJD) are commonly a comorbid condition with headaches. Studies have indicated that those suffering from myofascial related TMJD are more likely to suffer from chronic daily headaches, migraines, and tension-type headaches than those that do not experience TMJD pain. In most cases, the exact cause of TMJD is unclear; the National Institute of Dental and Craniofacial Research indicates that, regardless of the cause, researches will generally agree, the pathology will fall into three main categories:
- Myofascial pain involves discomfort or pain in the muscles that control jaw function
- Internal derangement of the joint involves a displaced disc, dislocated jaw, or injury to the condyle
- Arthritis refers to a group of degenerative/inflammatory joint disorders that can affect the temporomandibular joint
It is also possible that an individual may experience one or more of these at the same time. The pain experienced by most patients with a myofascial connection is concentrated around the masseter muscle and begins to spread towards the temporalis muscle. This deep and spreading pain is the primary symptom of patients diagnosed with myofascial TMJD pain.
While pain may be the primary symptom, TMJD can also present with muscle and/or joint pain, temporomandibular joint crepitus sounds, clicking, or popping (in the case of disc displacement or degenerative joint disorders); and restrictions, limitations, or deviation of the mandible when opening and closing the mouth.
Neuromuscular Therapy Treatments for TMJ Disorders
Typically, self-care or nonsurgical treatments are used to relieve temporary TMJD pain and discomfort. Surgery is a last resort if all conservative interventions have failed. Given that the majority of TMJD is myofascial in nature, a Neuromuscular Therapist is well suited to collaborate with Dentists and Orthodontists.
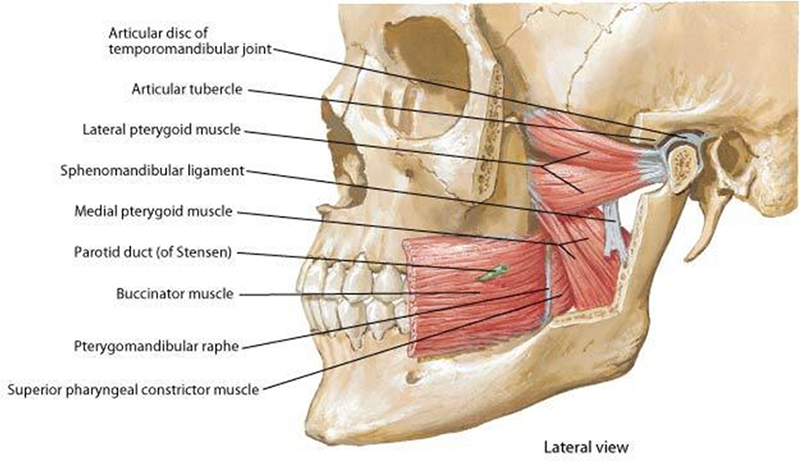
Lateral Temporomandibular Joint (TMJ) Muscles
When considering the musculature involved with TMJD Pain, a Neuromuscular Therapist would focus on:
- Lateral pterygoid
- Masseter (deep portion)
- Sternocleidomastoid (clavicular head)
- Medial pterygoid
In relation to headaches, these muscles would affect:
- Orbicularis oculi
- Temporalis (posterior fibers)
- Upper trapezius
- Occipitofrontalis
- Scalene
- Levator scapulae
- Splenius cervicis
Short-term & Long-term Management of TMJ Disorders
However, the difficulty of managing TMJD lies in the critical need to match the level of complexity of the management program with the complexity of the client’s condition. Also bear in mind the difference between temporarily relieving symptoms and correcting the cause of them.
It is vital for a Neuromuscular Therapist to identify appropriate short-term and long-term treatment goals for TMJD myofascial pain:
- Short-term goals:
- Reduce pain
- Restore muscle to normal length with full joint range of motion
- Restore muscle to normal posture
- Reduce sustained muscle activity and tension.
- Long-term goals:
- Restore normal lifestyle activities
- Reduce contributing and perpetuating factors
- Regular stretching, postural, and conditioning exercises
- Ongoing proper use of muscles.
The key to successful management lies in matching the client’s needs with a unique combination of active treatment, educational and contributing factors, and self-care appropriate for that client. For example:

Lateral Pterygoid Manual Therapy
- Visit one – Initial evaluation: history, examination, ordering of tests, imaging, and other consultations, provide self-care.
- Visit two – Comprehensive assessment: review test results, evaluation with neuromuscular therapist and health psychologist, review effects of self-care and other consultations, and discuss diagnosis, contributing factors, and treatment plan.
- Two or more visits as needed – Treatment program, 2 to 3 hour visits every 2 to 4 weeks for six months: neuromuscular therapy, exercises including postural, stretching, and relaxation, intraoral splint, anti-inflammatory and/or muscle relaxants, cognitive-behavioral therapy to address should factors.
- As needed – Follow-up care, one to two months as needed: continue exercises and splinting at night if needed, neuromuscular therapy if needed, and change contributing factors.
Evaluation of TMJD includes locating the trigger points in the muscles of the jaw and neck, as well as recognizing the contributing and perpetuating factors and correctly identifying the specific complexity of the case.

Medial Pterygoid Manual Therapy
- Management of TMJD involves selection of palliative care strategies, including the use of the stabilization splint, muscle exercises, OTC medications, and neuromuscular therapy treatments.
- Depending on the complexity of the case, cognitive-behavioral therapy with the health psychologist is included in the treatment plan, to reduce the contributing factors.
- The short-term goal is to restore the muscles to normal length, to improve posture, and to achieve full range of joint motion.
- The long-term goals include reducing the symptoms and negative effects while helping the client to return to normal function and minimizing the need for future care.
- The difficulty managing TMJD lies in the critical need to match the level of complexity of the management program with the complexity of the client. Failure to address the entirety of problems within a team approach in complex cases may lead to failure to resolve the pain and perpetuation of chronic pain syndrome.
DISCLAIMER | This article contains techniques taught in National Holistic Institute’s Advanced Neuromuscular Therapy Program and is for informational purposes only. Readers are advised to not attempt the techniques described without proper training. Doing so may result in serious physical injury. Please contact National Holistic Institute if you are interested in registering for classes.
Find out more about NHI’s Advanced Neuromuscular Therapy Program today. Complete this form to connect with an admissions representative.