A Neuromuscular Approach to Shin Splints

Manual Neuromuscular Therapy applied to Shin Splints
Shin Splints is a term that had been previously used to identify Medial Tibial Stress Syndrome (MTSS); according to “Principles of Athletic Training” 17th Edition by William E. Prentice, “shin splints” is currently used as an umbrella term that indicates pain in the anterior part of the shin. This pain can be caused by stress fractures, muscle strain, and acute or chronic anterior compartment syndromes. These injuries are typically attributed to repetitive stress and overuse.
Ida Rolf often said that stress works its way up the body. Given that theory, it is possible that a patient would experience a foot, ankle, or lower leg injury in their lifetime that the stress would work up to the knee, hip, low back, shoulder, neck, and ultimately, the head. As Neuromuscular Therapists approach a condition such as shin splints, it is important to understand these connections between where the patient is experiencing pain today and where it may have originated.
The question becomes, how do we differentiate the different aspects of anterior lower extremity pain?
Anterior Shin Splints
 Pain in the proximal anterior lateral region of the leg.
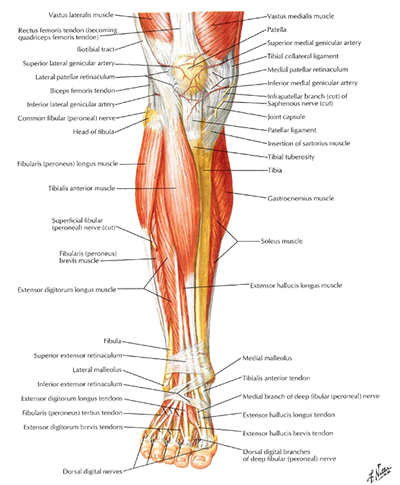
Pain in the proximal anterior lateral region of the leg.- This is attributed to excessive eccentric loading of the muscles that perform dorsiflexion such as, tibialis anterior, extensor digitorum longus, and extensor hallucis longus.
- The excessive eccentric loading may be caused by walking or running downhill. This constant tensile stress on the tibial attachment of the involved muscles produces irritation and inflammation of the periosteum.
- This can also be referred to as periostitis.
- Fascial tearing, ischemia, hypertonicity, or myofascial trigger points can also be components of anterior shin splints.
Posterior Shin Splints
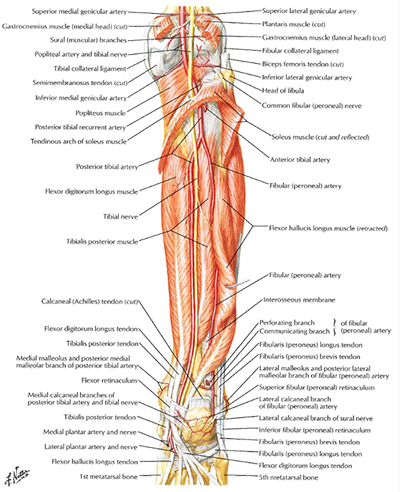 Majority of symptoms are felt at the distal 1/3 of the tibia where tibialis posterior and soleus attach.
Majority of symptoms are felt at the distal 1/3 of the tibia where tibialis posterior and soleus attach.- This is a stress reaction in the tibia due to chronic overloading.
- Frequently confused with tibial stress fractures.
- Patients are usually performing repetitive lower extremity activities such as jumping, running, (especially a forefoot running stride) or dancing.
- Other causes can include pes planus (flat feet), inadequate footwear, running on hard surfaces, improper biomechanical function of the foot or leg. These activities create a strong tensile load on the tibialis posterior which is transferred to the attachment site at the tibial border. As with anterior shin splints, the periosteum is stressed.
- Soleus may also play a role due to the close proximity of its attachment to tibialis posterior.
- Can be considered a warning sign for stress fractures in the tibia.
Compartment Syndrome
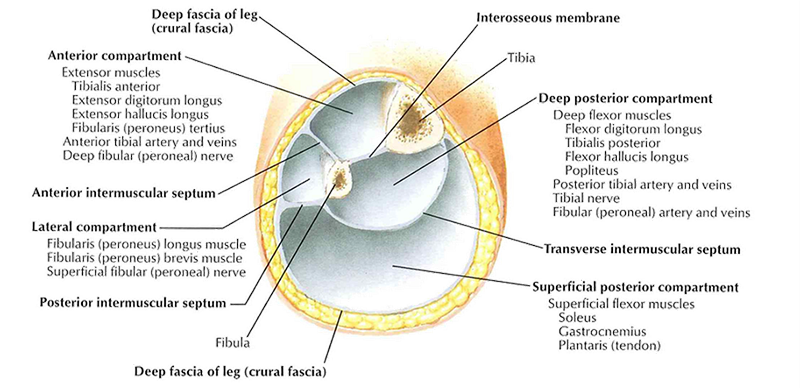
- Muscles are contained within fascial compartments; deep posterior, superficial posterior, lateral, and anterior. Each are separated by strong fascial walls that run through its length. These are stiff and less pliable than the fascial tissue in other regions of the body.
- Anterior Compartment Syndrome is caused by intra-compartmental pressure that increases due to muscular swelling. As muscles swell they compress other structures within the compartment causing neurovascular impairment.
- Anterior Compartment Syndrome is more prevalent as a chronic condition as a result from overuse. If it is chronic, it is referred to as exertional compartment syndrome.
- Overuse is typically related to running on a hard surface or sudden changes in training intensity.
Grades of Pain
When assessing the severity of shin splits, the patient is assessed within four grades of pain.
- Grade 1 – Pain after activity
- Grade 2 – Pain before and after activity with no effect on performance
- Grade 3 – Pain before, during, and after activity with an effect on performance
- Grade 4 – Pain so severe, performance is impossible
Within these four grades, the first two are typically due to overly shortened muscles that can be addressed with neuromuscular therapy. Grades three and four require a medical referral.
Unfortunately, there are no specific visual findings for anterior or posterior shin splints. A patient’s susceptibility to these conditions is likely if the patient exhibits flat foot or over pronation.
Range of Motion Observations
There are range of motion observations that will indicate the possibility of shin splints.
- Active Range of Motion – Dorsiflexion or plantar flexion may cause pain with either type of shin splint.
- Anterior Shin Splint – pain may occur during dorsiflexion or lengthening the anterior compartment in plantarflexion.
- Posterior Shin Splint – Pain may be felt during plantar flexion or stretching the posterior compartment by moving into dorsiflexion.
- An important consideration – pain may not occur until enough muscle fibers are recruited during the contraction or lengthening.
- Manual Resistive Testing – The same as active range of motion. Using MRT can help recruit enough muscle fibers to elicit a pain response.
- Passive Range of Motion – Anterior Shin Splints may be indicated if pain is produced at the far end of plantar flexion. Posterior Shin Splints may be indicated if pain is produce at the far end of dorsiflexion.
Pathologies That May Mimic Shin Splints
While assessing shin splints, Neuromuscular Therapists will have to eliminate other pathologies that can mimic these pain patterns. In collaboration with other health care providers, the following conditions must also be assessed:
- Stress fracture
- Proximal entrapment of the peroneal nerve
- Proximal neuropathy
- Lumbar radiculopathy
- Circulatory disorders
- Strain of the anterior compartment muscles
- Tenosynovitis
- Tendinitis
- Bone tumors

Because anterior shin splints and exertional anterior compartment syndrome occur often within the athletic population and their pain manifests on the anterior region of the shin, they are easily confused. Fortunately, there are notable differences. Compartment syndrome pain usually worsens as activity progresses and most of the pain is felt during the activity. Anterior shin splint pain can occur as activity beings, but will frequently subside as activity progresses. Pain from shin splints is routinely most aggravated a day or so after the activity has ended.
Neuromuscular Therapists should consider muscles associated with anterior leg pain, anterior ankle pain, and top of the foot pain. Another important factor to consider is the condition of the lumbar plexus and the sacral plexus. Given the motor innervation of the sciatic nerve to the musculature involved with shin splints, attention must also be given to a thorough hip assessment to determine the condition of the lumbopelvic structures. One must also consider the cutaneous or sensory innervation of the lumbar and sacral plexus to the area of the lower anterior portion of the leg.  A review of a dermatome chart indicates the L5 nerve root provides the sensory innervation to the portion of the leg where shin splint pain will typically manifest. The L5 nerve root can be aggravated by a herniated disc which can cause leg pain which can also be accompanied by numbness or other neurological symptoms. L5 supplies motor innervation to the muscles that raise the foot and big toe which can be observed by weakness in those muscles
A review of a dermatome chart indicates the L5 nerve root provides the sensory innervation to the portion of the leg where shin splint pain will typically manifest. The L5 nerve root can be aggravated by a herniated disc which can cause leg pain which can also be accompanied by numbness or other neurological symptoms. L5 supplies motor innervation to the muscles that raise the foot and big toe which can be observed by weakness in those muscles
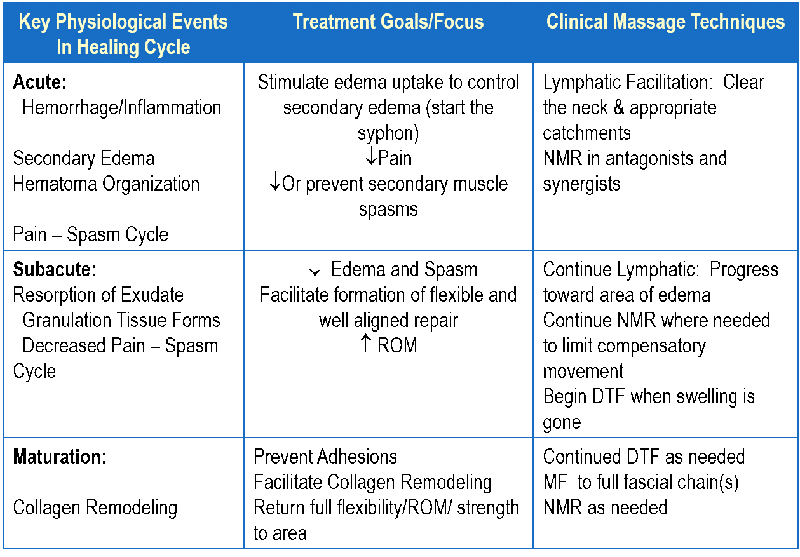
With each phase of the healing cycle, different goals are set to help the patient move efficiently through the healing process and certain manual therapy techniques can be applied. The following are general suggestions that can be applied to injuries; remember, specific techniques and duration of application will be dependent upon each patient’s ability to tolerate the treatment. Always collaborate with the appropriate health care provider before beginning any treatment plan.
 To learn how to thoroughly assess, strategize, and collaborate on an effective treatment plan for shin splints, enroll in the Advanced Neuromuscular Therapy Program on a National Holistic Institute | A College of Massage Therapy Campus near you.
To learn how to thoroughly assess, strategize, and collaborate on an effective treatment plan for shin splints, enroll in the Advanced Neuromuscular Therapy Program on a National Holistic Institute | A College of Massage Therapy Campus near you.
DISCLAIMER | This article contains techniques taught in National Holistic Institute’s Advanced Neuromuscular Therapy Program and is for informational purposes only. Readers are advised to not attempt the techniques described without proper training. Doing so may result in serious physical injury. Please contact National Holistic Institute if you are interested in registering for classes.
Find out more about NHI’s Advanced Neuromuscular Therapy Program today. Complete this form to connect with an admissions representative.