What You Need to Know About Frozen Shoulder and Neuromuscular Therapy
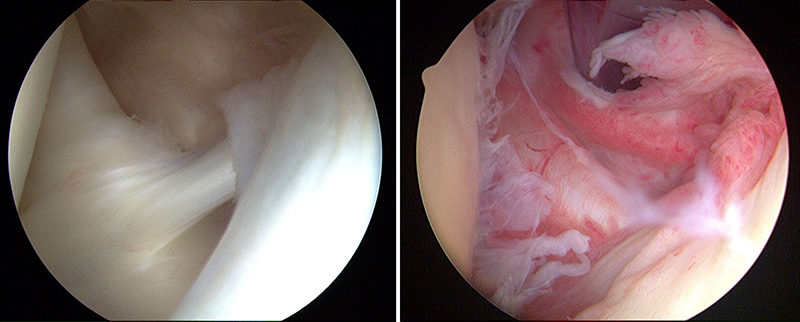
Frozen Shoulder (photo credit)
Shoulder pain is the third most prevalent reason consumers seek Massage Therapy. When considering the incredible mobility of the glenohumeral joint, losing function due to movement reduction and/or pain can create incredible obstacles in our daily lives. There are several terms used to describe shoulder mobility limitations/pain including arthritis, bursitis, Frozen Shoulder, and Adhesive Capsulitis. “The incidence of adhesive capsulitis in the general population is approximately 3% to 5% but as high as 20% in patients with diabetes. Idiopathic adhesive capsulitis often involves the nondominant extremity, although bilateral involvement has been reported in up to 40% to 50% of cases.”1 Typically, Frozen shoulder is seen more in women, diabetic patients, and between the ages of 50 – 70.
What is Frozen Shoulder?
“Frozen shoulder, also referred to as adhesive capsulitis, is a common condition affecting the glenohumeral joint characterised by progressive inflammation of the joint capsule and subsequent stiffness of the shoulder…The term frozen shoulder has in the past been used inaccurately as a general diagnosis for shoulder pain and stiffness…Precise definitions of this condition vary, as the aetiology, pathophysiology, and treatment are subjects of continued debate.”2 Because of the debate surrounding its etiology, “Adhesive capsulitis is a syndrome defined in its purest sense as idiopathic painful restriction of shoulder movement that results in global restriction of the glenohumeral joint…To avoid confusion, the term “adhesive capsulitis” should be used to refer to the primary idiopathic condition and the term “secondary adhesive capsulitis” should be applied to the condition that is associated with, or results from, other pathologic states.”3
Adhesive capsulitis, or the primary idiopathic condition usually presents as a gradual onset and slow development of symptoms and lack any specific mechanism of injury. Whereas the frozen shoulder, or secondary condition have experienced trauma or prolonged immobilization. There appears to be a strong correlation of adhesive capsulitis with diabetes mellitus. “It is believed that in patients with diabetes, associated microvascular disease causes abnormal collagen repair, which predisposes them to adhesive capsulitis.”3
It is incredibly difficult to differentiate adhesive capsulitis from frozen shoulder and other glenohumeral pathologies. Many of the pathologies have similar signs, symptoms, etiologies, and mechanisms of injury. Typically, one will find pain and limitations in active range of motion and passive range of motion. Conducting an appropriate HOPRS assessment will help determine the source of the shoulder guarding the patient is experiencing which will lead to an efficient and effective multi-session strategy of care.
Immobilization is mentioned as a potential contributor to frozen shoulder. The immobility or reduced mobility can be the result of a rotator cuff injury, broken arm, stroke, or recovery from surgery.4 A concern from surgical procedures can stem from mastectomies performed in response to breast cancer.
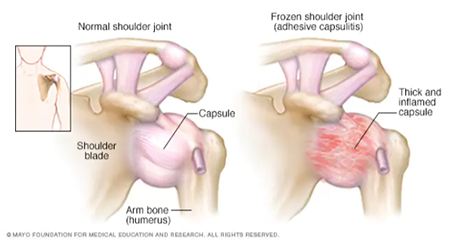
Normal Shoulder Joint vs Frozen Shoulder Joint
Three Stages to Determine the Progression of Frozen Shoulder
- Freezing stage – Any movement of your shoulder causes pain, and your shoulder’s range of motion starts to become limited.
- Frozen stage – Pain may begin to diminish during this stage. However, your shoulder becomes stiffer, and using it becomes more difficult.
- Thawing stage – The range of motion in your shoulder begins to improve.4
In total, the three stages can last up to two years. The freezing stage may be present for approximately three months; while the frozen stage can be experienced for 3-9 months, and the thawing stage can take anywhere between 9-18 months.
Neuromuscular Considerations for Frozen Shoulder
External rotation of the glenohumeral joint is the first range of motion lost with frozen shoulder. This symptom correlates with trigger point findings when the subscapularis muscle exhibits active trigger points which makes it the most important muscle to address in frozen shoulder. The main goal for treatment is to maintain and restore pain-free motion. Typically, in the freezing stage, pain is the main restricting factor of movement. The pain is generated from the soft tissue structures and according to “Travell, Simons, & Simons’ Myofascial Pain and Dysfunction” 3rd edition, “painful spasm of the subscapularis, with TrPs, accompanies frozen shoulder from the onset.” Another consideration is the relationship of the subscapularis tendon with the subscapular bursa. If the bursa is involved with frozen shoulder, the inflammation to that bursa could be caused by compression and friction from the subscapular tendon which creates fibrotic tissue in the bursa as a protective response. This fibrous tissue limits the bursa’s function which can lead to movement limitations.
Aside from the subscapularis, the other rotator cuff muscles can also be involved and when reviewing their pain referral patterns, one can see a correlation to the movement avoidance due to pain. Keep in mind the main function of the rotator cuff muscles is to stabilize the humerus in the glenoid fossa. Without appropriate joint alignment, efficient movement of the glenohumeral joint is not possible and potentially painful.
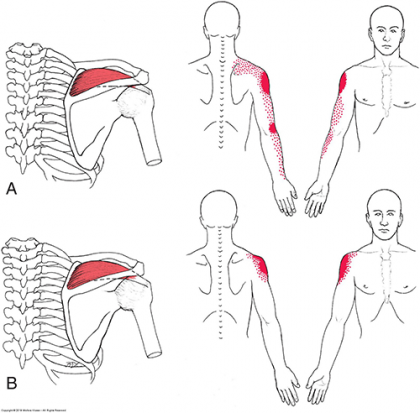
Supraspinatus Muscle and its Pain Referral Patterns
Supraspinatus
- Action/Function
- Large initiator of shoulder abduction
- External rotation with 90° abduction
- Prevents downward displacement of the humerus
- Dynamic stabilizer of the glenohumeral joint during activity
- Symptoms
- Lateral shoulder pain that may spread distally to the lateral epicondyle of the humerus
- Pain at the glenohumeral joint especially during initiation of abduction
- Deep, dull ache in the lateral shoulder at rest
Infraspinatus
- Action/Function
- External rotation at the glenohumeral joint
- Dynamic stability of the glenohumeral joint
- Stabilize the head of the humerus in the glenoid fossa during upper extremity movement
- Prevents anterior/posterior subluxation of the glenohumeral joint
- Symptoms
- Pain at rest that can also interfere with sleep
- Deep ache in the anterior shoulder
- Pain on the medial border of the scapula at the rhomboid attachment
- Inability to medially rotate and adduct the arm and glenohumeral joint simultaneously
Teres Minor
- Action/Function
- Prime mover of the glenohumeral joint in lateral rotation
- Dynamic stability of the glenohumeral joint
- Resists upward shear forces of the deltoid during shoulder elevation
- Symptoms
- Pain can be confused with bursitis pain
- Primary concern is posterior shoulder pain
Subscapularis
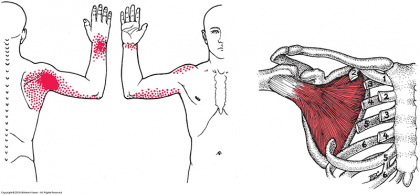
Subscapularis Muscle and its Pain Referral Patterns
- Action/Function
- Medially rotates the humerus
- Dynamic stability to the glenohumeral joint
- Stabilize the head of the humerus during upper extremity movement
- Prevents anterior displacement of the humeral head
- Symptoms
- Difficulty and pain lifting the arm
- Inability to reach the opposite armpit
- Snapping or clicking sounds around the shoulder with movement
- Frozen shoulder
Neuromuscular therapy can be an effective treatment during the freezing stage of frozen shoulder. With some patients experiencing movement disruptions for up to 10 years after the thawing phase, re-establishing normal glenohumeral joint function is crucial to recovery. Neuromuscular Therapists should collaborate with physical therapists, chiropractors, and medical physicians to fully address their patient’s needs in relation to frozen shoulder.
1Adhesive Capsulitis of the Shoulder: Review of Pathophysiology and Current Clinical Treatments
2The Frozen Shoulder: Myths and Realities
3Adhesive Capsulitis: A Sticky Issue
DISCLAIMER | This article contains techniques taught in National Holistic Institute’s Advanced Neuromuscular Therapy Program and is for informational purposes only. Readers are advised to not attempt the techniques described without proper training. Doing so may result in serious physical injury. Please contact National Holistic Institute if you are interested in registering for classes.
Get the details about NHI’s Advanced Neuromuscular Therapy Program and its value in restoring function and addressing chronic pain today. Complete this form to connect with an admissions representative.