A Neuromuscular Therapy Approach to Lateral Ankle Sprains

ANMT Program Founder Cynthia Ribeiro working on the lateral leg
Overview of Lateral Ankle Sprains
In regards to sports injuries, the ankle is one of the most commonly injured. “Lateral ankle sprains (LASs) are often considered a benign injury with no lasting consequences.
However, at least one-third of individuals who sustained an LAS will experience residual symptoms. These symptoms, often termed ‘chronic ankle instability’ (CAI), can significantly alter an individual’s health and function by causing him or her to become less active over their life span.”1 It has been found that “approximately 25% of those who sprain their ankles are unable to attend school or work for at least 1 week.”1
To help us better understand approaches to supporting rehabilitation from lateral ankle sprains we’re going to discuss the anatomical structures involved in a lateral ankle sprain.
Ligaments Involved in Lateral Ankle Sprains
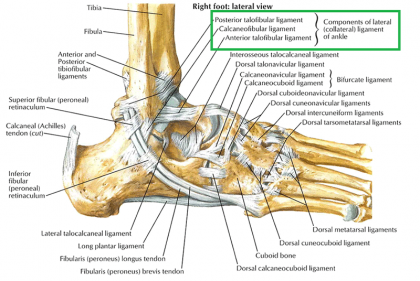
Lateral Ankle Ligament – Netter Plate 527
There are 3 main ligaments involved in varying degrees of ankle sprains. They are the Anterior Talofibular Ligament (ATFL), the Calcaneofibular ligament (CFL), and the Posterior Talofibular Ligament (PTFL); all three of these ligaments comprise the Lateral Collateral Ligament of the ankle.
The ATFL functions to resist inversion and plantar flexion of the ankle; it is the weakest of the lateral collateral ligaments and will be the first to get injured. The ATFL is generally the only ligament affected in a Grade 1 Lateral Ankle Sprain because the most common mechanism of injury, (MOI) in a lateral ankle sprain is plantar flexion and inversion which are the two forces that the ATFL prevent.
The CFL is the middle ligament of the lateral collateral ligament complex and will provide lateral stability to the ankle joint and the subtalar joint. The CFL is a primary restraint to inversion at the talocrural joint and it is generally unaffected with a Grade 1 Lateral Ankle Sprain.
The PTFL is important for stability when the ankle is dorsiflexed and is minimally affected by ankle inversion; this leads us to conclude that the PTFL resists posterior displacement of the calcaneus. Generally, Grade 2 and Grade 3 lateral ankle sprains will affect the CFL and the PTFL.
Muscles Involved in Lateral Ankle Sprains
While sprains typically involve damage to the ligaments, Neuromuscular Therapists must also consider the affect this injury has on the musculature. We are observing a disruption to the stability of the ankle joint and when the main stabilizing structures are affected, the musculature has to increase its activity to provide additional stability.
Simultaneously, the musculature that crosses the ankle are over-lengthened during a lateral ankle sprain and must be rehabilitated. Failure to properly rehabilitate all structures following a lateral ankle sprain can lead to a lifetime of ankle instability. Given that the primary mechanism of injury of a lateral ankle sprain is plantar flexion and inversion, the musculature that would be involved function to control those ranges of motion with their eccentric contraction.
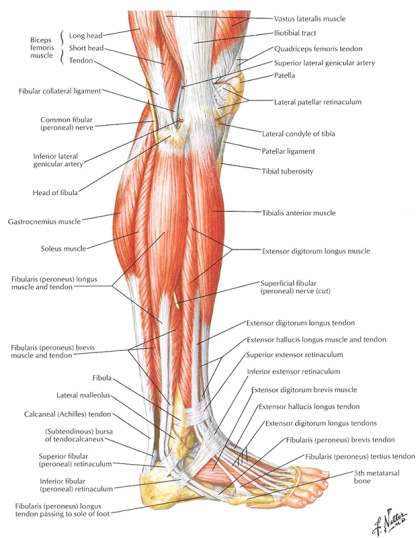
Lateral Leg Muscles – Netter Plate 521
The muscles in the lateral compartment of the leg are Fibularis Longus and Fibularis Brevis. In an open kinetic chain, these muscle produce eversion of the ankle. The Fibularis Longus will also produce plantar flexion of the foot in an open and closed kinetic chain. While their action, or concentric contraction is important, their function, or eccentric contraction is where we will focus.
Studies have shown that the Fibularis Longus and Brevis will depress or fix the medial margin of the foot to contact the surface during weight-bearing activities to resist inadvertent or excessive inversion of the ankle. If a patient does experience a lateral ankle sprain, these muscles will eccentrically contract to prevent that motion and then eventually, with enough force, damage will occur.
Taking into consideration their role in gait, the Fibularis Longus and Brevis work together to control the transition from inversion at the early stance phase to a neutral position at the mid-stance phase.
Additionally, individuals with flat feet experience hypermobility in the foot and the Peroneus Longus and Brevis are more active in those individuals. An interesting phenomenon is that the Peroneus Longus and Brevis aren’t as active when stabilizing the foot when the individual is not wearing shoes.
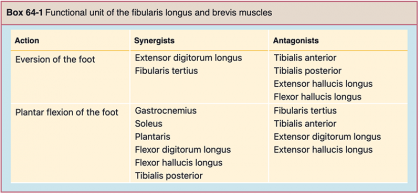
Box 64-1 – Travell, Simons & Simons’ Myofascial Pain and Dysfunction – The Trigger Point Manual 3rd Ed. Pg.678
Earlier we mentioned, the primary MOI are inversion and plantar flexion. To consider all the muscles that control those motions, we will look at the opposing movements of eversion and dorsiflexion. The chart indicates the muscles that will be involved and the manner in which they should be addressed will be discussed in Part 2 of this blog.
It is important for us to remember that the modalities we can apply during an acute injury and the inflammatory response phase of healing are mainly targeted to reduce hematoma and prevent secondary tissue damage. While the primary site may be off limits to most massage modalities, we can definitely work with the synergists and antagonists of the functional unit as long as they aren’t injured as well. This means we must consider the degree of the injury to determine the extent of the tissue damage and collaborating with the appropriate health care providers will give us the necessary diagnosis to safely proceed with our strategies.
1“Incidence and Cost of Ankle Sprain in United States Emergency Departments” Shweta Shah, et al.
DISCLAIMER | This article contains techniques taught in National Holistic Institute’s Advanced Neuromuscular Therapy Program and is for informational purposes only. Readers are advised to not attempt the techniques described without proper training. Doing so may result in serious physical injury. Please contact National Holistic Institute if you are interested in registering for classes.
To learn more about Neuromuscular Therapy applied to the lower extremity, contact an Admissions Representative to begin classes in Emeryville, San Jose, Studio City, and Santa Ana in February 20222.
Get the details about NHI’s Advanced Neuromuscular Therapy Program today. Complete this form to connect with an Admissions Representative.