Neuromuscular Therapy and Headache Management for the Most Prevalent Types of Headaches
June is National Migraine & Headache Awareness month. In an effort to increase awareness, Phil Okazaki, Senior Advanced Neuromuscular Therapy Program Instructor from the San Jose Campus has provided a list of the most prevalent headaches and how Neuromuscular Therapists assist patients in the management of the associated discomfort from migraines and headaches.
Headaches are one type of pain that people feel is “normal.” Most of the attention has been focused on four of the most prevalent types of headaches.
- Tension Type Headache (TTH)
- Cervicogenic Headache
- Migraine Headache without Aura
- Myogenic Headache
The most common form of headache is the Tension Type Headache; it is also the most often neglected. “Functional and work disability has been described by 60% of patients with headache and accounted for 64% of the reduction in working capacity due to head pain.” Let’s take a closer look at each of the most prevalent types.
Migraine and TTH episodes show significant changes in serotonin levels. Serotonin is a neurotransmitter that has been implicated in a number of central nervous system disorders. The changes in serotonin activity may lead to the dilation of arteries in the periphery of the brain. The excessive vasodilation stretches blood vessels, causing pain. Additionally, prostaglandin release may initiate an inflammatory response which adds to the fluid in the closed cavity of the cranium.
TENSION TYPE HEADACHE
These can last from 30 minutes to 7 days and have at least two of the following features:
- Bilateral location
- Pressing and tightening pain quality
- Mild or moderate pain intensity
- Lack of aggravation during routine physical activity
The discomfort of TTH is similar to a band squeezing the head. There is a lot of debate over the pathophysiology of TTH. The predominant theory historically has been that TTH are due to sustained contraction of the cervical and pericranial muscles. Myofascial trigger point activity dramatically increases in response to psychological stress and diminishes with relaxation; it has been observed that TTH worsen with stress and improve with relaxation.
 When considering the anatomy involved with TTH; the average head weighs about 15-18 pounds. The occipital condyles and facets of C1 have a similar surface area as touching two fingertips together. This mechanism is kept in balance by tension exerted by muscles and ligaments around the neck and head; the muscles responsible for the posture of the head form two inverted triangles just below the occiput. It is not surprising that when this delicate balance is disturbed the resulting pain reverberates throughout the entire structure. Additionally, postural and movement patterns in other parts of the body exert force on the spine which can result in tension at this delicate occipital connection. For example, when a foot strikes the ground too hard on the lateral side, it may pull on the knee which then demands compensation at the hip. The sacrum then must adjust to the pelvis which creates a slight twist in the lumbar vertebra; this force is then transmitted up the spine to the head.
When considering the anatomy involved with TTH; the average head weighs about 15-18 pounds. The occipital condyles and facets of C1 have a similar surface area as touching two fingertips together. This mechanism is kept in balance by tension exerted by muscles and ligaments around the neck and head; the muscles responsible for the posture of the head form two inverted triangles just below the occiput. It is not surprising that when this delicate balance is disturbed the resulting pain reverberates throughout the entire structure. Additionally, postural and movement patterns in other parts of the body exert force on the spine which can result in tension at this delicate occipital connection. For example, when a foot strikes the ground too hard on the lateral side, it may pull on the knee which then demands compensation at the hip. The sacrum then must adjust to the pelvis which creates a slight twist in the lumbar vertebra; this force is then transmitted up the spine to the head.
Some of the major causes of TTH can include:
- Trigger points in the muscles of the head and neck
- Ongoing emotional, mental, or physical stress
- Worry and anger typically trigger clenched jaws and neck tension
- Muscular or ligamentous injury to the head and neck strucutres
- Structural problems – misalignment of the cranial bones and Temporomandibular joint
- Eyestrain
CERVICOGENIC HEADACHE
 The American Migraine Foundation’s definition states: “referred pain (pain perceived as occurring in a part of the body other than its true source) perceived in the head from a source in the neck.” They are characterized by:
The American Migraine Foundation’s definition states: “referred pain (pain perceived as occurring in a part of the body other than its true source) perceived in the head from a source in the neck.” They are characterized by:
- Generalized unilateral pain
- Moderate to severe pain intensity
- Non-throbbing or non-lancinating pain quality
- Restriction of the typical neck range of motion
- High probability of myofascial trigger point pain
In addition to these characteristics, the head pain is typically increased by head movement, maintained neck postures, or external pressure over the cervical joints.
MIGRAINE HEADACHE WITHOUT AURA
The word “migraine” is derived from the French word, “hemicrane,” or half-head because the characteristic pain presentation is half of the head. These typically last from 4 – 72 hours and have at least two of the following features:
- Unilateral location
- Pulsating pain quality
- Moderate or severe pain intensity
- Aggravation by routine activities
- Associated with phonophobia or photophobia
- Nausea
- High probability of myofascial trigger point pain
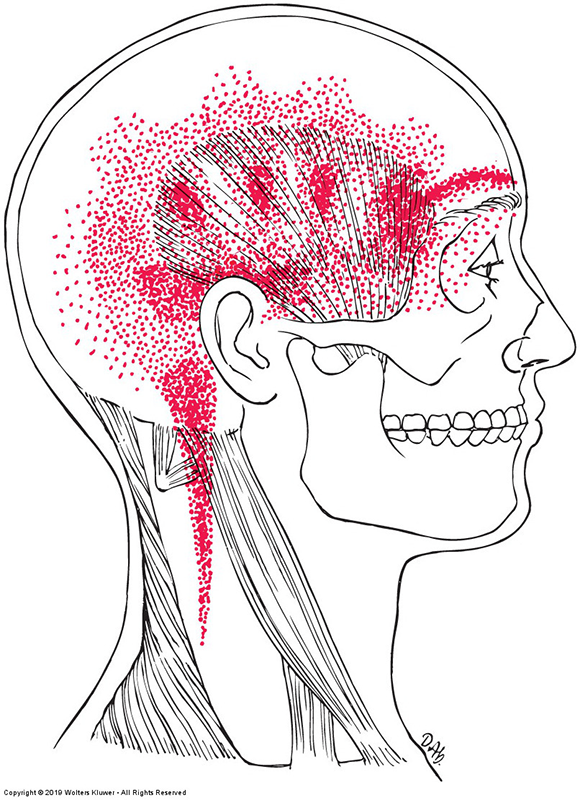
Migraine without aura can also be termed a common migraine. These have been shown to have focal, cervical, and masticatory muscle tenderness with associated referred symptoms that reproduced or caused headache pain. Typically, these pericranial muscle sites are more tender in migraine patients than non-headache even when the migraine patient is headache-free. Overlapping pain referral patterns from myofascial trigger points in various pericranial muscles produce atypical migraine symptoms that can be unilateral or bilateral.
Pain generated by TTH, cervicogenic, and migraine without aura typically have a steady, deep, aching pain which is very similar to the discomfort experienced from trigger points. The pain can also be referred to and from the cervical spine. “A recent study found a prevalence of neck pain of 89.3% in patients with migraine combine with TTH, 88.4% in those with TTH, and 76.2% in those with migraine.
It is also possible for people to experience two types of headaches simultaneously. If these headaches are triggered by pain referred from trigger points, they can be called myogenic, (beginning in the muscle) headaches.
MYOGENIC HEADACHE
 These headaches involve a significant component of pain referred from trigger points. Therapists working with these muscles must go back and forth between active trigger point therapy and the area of referral to apply specific point work.
These headaches involve a significant component of pain referred from trigger points. Therapists working with these muscles must go back and forth between active trigger point therapy and the area of referral to apply specific point work.
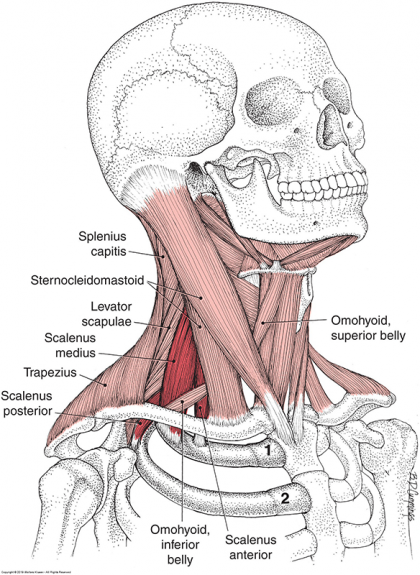
When considering headache treatment through Massage Therapy, the Therapist should consider “muscles innervated by C1-C3 or the trigeminal nerve should be explored for the presence of trigger points.” Those muscles include:
- Upper Trapezius
- Sternocleidomastoid
- Masseter
- Splenius Capitis
- Splenius Cervicis
- Semispinalis Capitis
- Temporalis
- Levator Scapulae
- Suboccipital muscles
- Superior Oblique muscles
Some have theorized that patients can be misdiagnosed as having migraines when trigger points are the problem. This theory is based on the effects trigger points can have on the trigeminal nerve. If there are trigger points in muscles innervated by the trigeminal nerve, the resulting nociceptive signal can precipitate, perpetuate, or aggravate migraines.
DISCLAIMER | This article contains techniques taught in National Holistic Institute’s Advanced Neuromuscular Therapy Program and is for informational purposes only. Readers are advised to not attempt the techniques described without proper training. Doing so may result in serious physical injury. Please contact National Holistic Institute if you are interested in registering for classes.
Do you have questions about the Advanced Neuromuscular Therapy Program? Complete this form to connect with an admissions representative today.